Colon Cancer
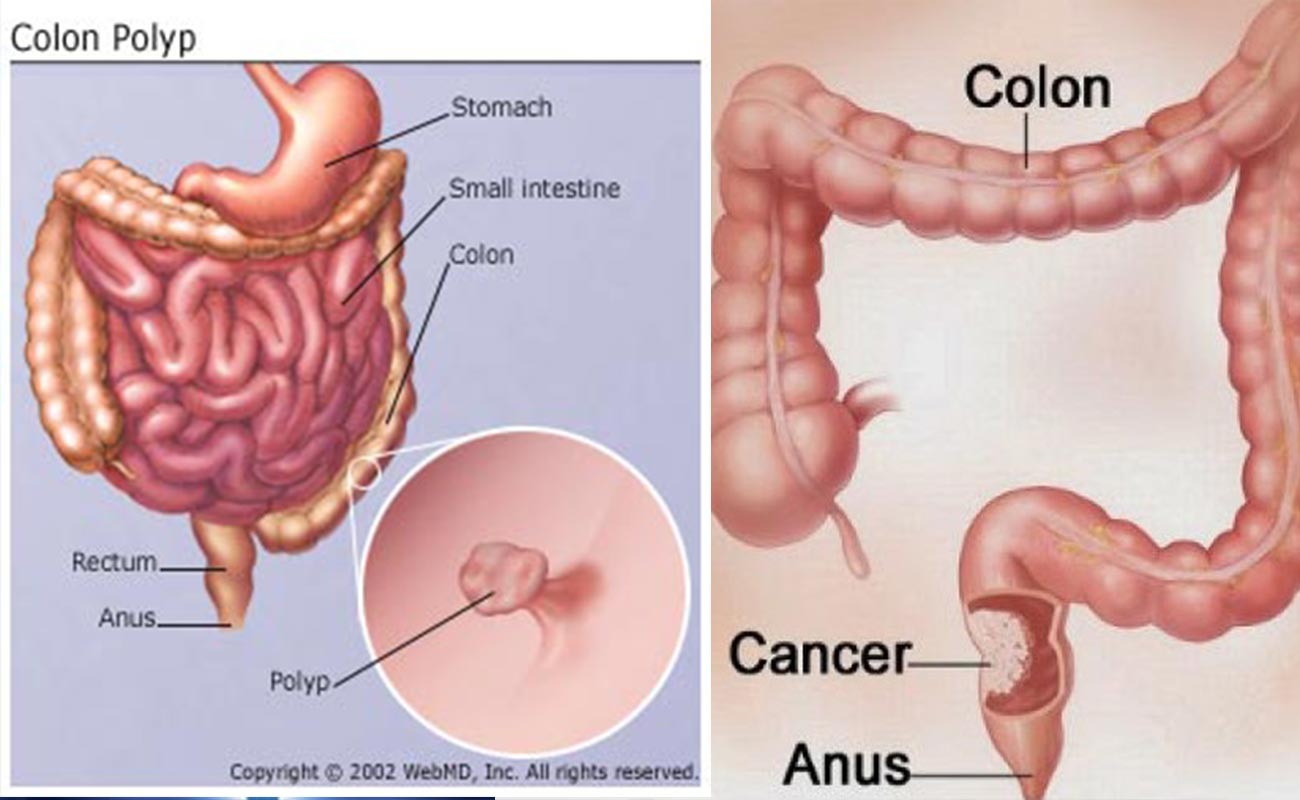
Colon or in another term, the large intestine, is the lowest part of the digestive system. Inside the colon, water and salt from solid wastes are extracted before the waste moves through the rectum and exits the body through the anus.
Cancer is a class of diseases characterized by out-of-control cell growth. Most colon cancers originate from small, noncancerous (benign) tumors called adenomatous polyps that form on the inner walls of the large intestine.
Some of these polyps may grow into malignant colon cancers over time if they are not removed during colonoscopy - a procedure looking at the inner lining of the intestine.
Colon cancer cells will invade and damage healthy tissue that is near the tumor, causing many complications.
Excluding skin cancers, colorectal cancer is the third most common cancer diagnosed in both men and women in the United States. The American Cancer Society’s estimates for the number of colorectal cancer cases in the United States for 2017 are:
Colorectal cancer is the third leading cause of cancer-related deaths in women in the United States and the second leading cause in men. It is expected to cause about 50,260 deaths during 2017.
Symptoms
Signs and symptoms of colon cancer include:
Talk to your doctor about when you should begin screening for colon cancer. Guidelines generally recommend that colon cancer screenings begin at age 50. Your doctor may recommend more frequent or earlier screening if you have other risk factors, such as a family history of the disease.
Causes
The most common forms of inherited colon cancer syndromes are:
Diagnosis
In order to diagnose colon cancer, physicians will request a complete physical exam as well as personal and family medical histories. Diagnoses are usually made after the physician conducts a colonoscopy or a barium enema x-ray.
Prognosis
After a diagnosis is made, doctors determine the stage of the cancer. The stage determines which choices will be available for treatment and informs prognoses.
The standard cancer staging method is called the TNM system:
Factors that may increase your risk of colon cancer include:

Cancer treatment depends on the type of cancer, the stage of the cancer (how much it has spread), age, health status, and additional personal characteristics. There is no single treatment for cancer, but the most common options for colon cancer are surgery, chemotherapy, and radiation therapy.
Treatments seek to remove the cancer and/or relieve painful symptoms that the cancer is causing.
Surgery to remove part of or the entire colon is called colectomy. During colectomy, a surgeon will remove the part of the colon containing the cancer as well as the marginal area close to the cancer.
Also, nearby lymph nodes are also usually removed. Depending on the extent of the colectomy, the healthy portion of the colon will either be reattached to the rectum or attached to an opening in the wall of the abdomen called a stoma. This latter option is called a colostomy, and waste will exit the body through the stoma into a colostomy bag, instead of exiting through the rectum.
In addition to invasive surgeries like colectomy, doctors can remove some small, localized cancers using endoscopy.
Laparoscopic surgery (using several small incisions in the abdomen) may also be an option to remove larger polyps.
Palliative surgery might also be employed to relieve symptoms for cancers that are advanced or untreatable. This type of surgery will try to relieve blockage of the colon or to inhibit other conditions to relieve pain, bleeding, and other symptoms.
Chemotherapy utilizes chemicals that interfere with the cell division process - damaging proteins or DNA - so that cancer cells will become damaged and die. These treatments target any rapidly dividing cells (not necessarily just cancer cells), but normal cells can usually recover from any chemical-induced damage, while cancer cells cannot.
Chemotherapy is generally used to treat cancer that has spread or metastasized because the medicines travel throughout the entire body. Treatment occurs in cycles so the body has time to heal between doses. However, there are still common side effects such as hair loss, nausea, fatigue, and vomiting. Combination therapies often include multiple types of chemotherapy or chemotherapy combined with other treatment options.
One large-scale study has shown that daily low-dose aspirin improves the survival of patients with certain gastrointestinal cancers, such as colon cancer. While the mechanism is not well understood and aspirin's role in prevention has not been well studied, this information provides another possible adjunctive treatment option.
Radiation treatment, also known as radiotherapy, destroys cancer by focusing high-energy rays on the cancer cells. This causes damage to the molecules that make up the cancer cells and leads them to die.
Radiotherapy uses high-energy gamma-rays that are emitted from metals such as radium or high-energy x-rays. Radiotherapy can be used as a standalone treatment to shrink a tumor or destroy cancer cells; it is also used in combination with other cancer treatments.
Radiation treatments are not often used for early stage colon cancers, but may be employed if early stage rectal cancer has penetrated the wall of the rectum or traveled to nearby lymph nodes.
Side effects of radiation therapy may include mild skin changes resembling sunburn or suntan, nausea, vomiting, diarrhea, and fatigue. Patients also tend to lose their appetites and have trouble maintaining weight, but most side effects subside a few weeks after completing treatment.
Colon cancer is the third most common cause of cancer death in the U.S., and it is the second most prevalent type of cancer. Regular annual screening for both men and women aged 50 to 75 years is recommended by the U.S. Preventive Task Force.
The American Cancer Society suggests screening tests, particularly colonoscopy, for early detection of colon cancer. Colonoscopy is the best method, because it will visualize the entire colon and can remove polyps during the procedure. Other screening tests include fecal occult blood tests (annually), stool DNA testing, flexible sigmoidoscopy (every 5 years), and CT colonography (every 5 years).
These frequency recommendations depend, however, on a person's particular risk of colon cancer due to other risk factors.
In general, physicians recommend standard preventive measures such as keeping a healthy weight, exercising, and increasing consumption of fruits, vegetables, and whole grains while decreasing saturated fat and red meat intake. In addition, people are recommended to limit alcohol consumption and quit smoking.
Dr. Felice Schnoll-Sussman, a gastroenterologist from the NewYork-Presbyterian/Weill Cornell Medical Center, said that it is important for people to realize that with proper screening, colon cancer cannot only be detected early, but may also be prevented from developing.
Sources: medicalnewstoday, mayoclinic, cancer.org
Submit Comment