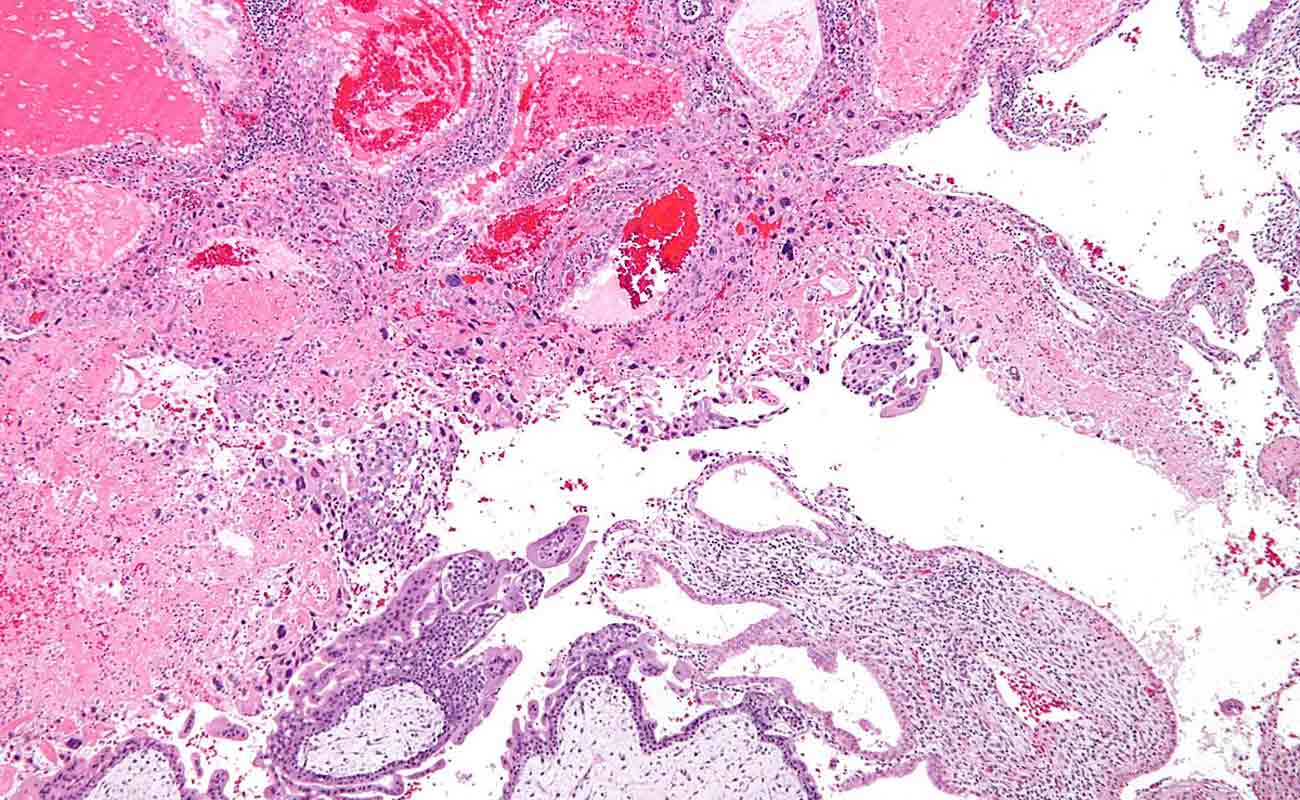
Molar pregnancy is an abnormal form of pregnancy in which a non-viable fertilized egg implants in the uterus and will fail to come to term. A molar pregnancy is a gestational trophoblastic disease which grows into a mass in the uterus that has swollen chorionic villi. These villi grow in clusters that resemble grapes. A molar pregnancy can develop when a fertilized egg does not contain an original maternal nucleus. The products of conception may or may not contain fetal tissue. It is characterized by the presence of a hydatidiform mole (or hydatid mole, mola hydatidosa). Molar pregnancies are categorized as partial moles or complete moles, with the word mole being used to denote simply a clump of growing tissue, or a growth.

Complete molar pregnancies have only placental parts (there is no baby) and form when the sperm fertilizes an empty egg. Because the egg is empty, no baby is formed. The placenta grows and produces the pregnancy hormone, hCG. Unfortunately, an ultrasound will show that there is no fetus, only a placenta.
A molar pregnancy may seem like a normal pregnancy at first, but most molar pregnancies cause specific signs and symptoms, including:
If you experience any signs or symptoms of a molar pregnancy, consult your doctor or pregnancy care provider. He or she may detect other signs of a molar pregnancy, such as:
A risk factor is anything that can increase your chance of developing a disease or condition. Each condition has different risk factors. Researchers have not yet been able to identify what causes molar pregnancies, but we do know of some factors that increase a woman's risk of developing this type of tumor.
Remember that having a risk factor does not mean that you will definitely get a particular medical condition. Most women who have one or more risk factors never develop a molar pregnancy, and some people who have none of the risk factors do develop one. This is only a guide to what may increase risk. Gestational trophoblastic tumors are rare. In the UK, there is about 1 molar pregnancy for every 590 pregnancies.
A risk factor is anything that can increase your chance of developing a disease or condition. Each condition has different risk factors. Researchers have not yet been able to identify what causes molar pregnancies, but we do know of some factors that increase a woman's risk of developing this type of tumour.
Remember that having a risk factor does not mean that you will definitely get a particular medical condition. Most women who have one or more risk factors never develop a molar pregnancy, and some people who have none of the risk factors do develop one. This is only a guide to what may increase risk. Gestational trophoblastic tumours are rare. In the UK, there is about 1 molar pregnancy for every 590 pregnancies.
Molar pregnancy is an abnormal pregnancy, so all women who become pregnant have a slight risk of developing it. However, researchers have found that some types of molar pregnancy are more common in certain age groups. Complete molar pregnancies are more common in teenage mothers and mothers over the age of 45. But age does not affect the risk of partial molar pregnancies.
Molar pregnancies are more common in women from Asian countries than in those from other ethnic groups.
If you have already had one molar pregnancy, you have about a 1 in 100 chance (1%) of having another one. This means that 99 out of every 100 women (99%) who become pregnant after a molar pregnancy will have a normal pregnancy. If you have had two or more molar pregnancies your risk of having another is higher, at about 15 to 20 out of 100 (15 to 20%).
In most cases, molar pregnancy is discovered when a miscarriage occurs. If a molar pregnancy is suspected before a miscarriage occurs, it can usually be detected by ultrasound.
Blood and urine tests may be used to detect abnormally high levels of human chorionic gonadotropin (hCG). This is a hormone normally produced during pregnancy but present at much higher levels with molar pregnancy.
Although any woman who becomes pregnant is at some risk of developing one of these uncommon conditions, the risk appears to be higher in pregnant women who are younger than age 20 or older than age 40.
The best way to prevent complications from an invasive mole or a choriocarcinoma is to receive routine prenatal care by a qualified health care professional, so that problems can be identified as early as possible.
The results of diagnostic tests will help to determine a treatment plan. Options for treatment almost always include surgery to remove the tumor. More aggressive types of molar pregnancy may require chemotherapy and/or radiation therapy. About 85% of hydatidiform moles can be treated without chemotherapy. Treatment options include:

Follow-up of every woman who has had a molar pregnancy is mandatory, whether partial or complete. This is because of the risk of developing a gestational trophoblastic tumor or neoplasm (GTN), which is the cancerous form of GTD. The focus of follow-up is to confirm that treatment is successful and identify persistent GTD or GTN.
Follow-up should include regular blood hCG testing and asking about symptoms such as irregular bleeding from the uterus. The hCG level is usually above 100 000 IU/L in a complete mole, but may be normal or slightly raised in a partial mole. Following evacuation, the hCG level falls dramatically within a couple of days, to the normal level of a non-pregnant woman. When this drop fails to occur, or a rise is seen, persistent GTD is diagnosed.
Persistent GTD occurs after a partial mole in 0.1-4% of women, but metastasis is very rare. It is most likely to arise within 12 months of evacuation, and most commonly within 6 months.
After a complete mole is evacuated, the risk of persistent GTD is 5 times higher. This risk drops somewhat following a hysterectomy.
Weekly testing of this hormone will alert one to the possibility that GTN has developed because the hCG level will fail to drop, or will continue to rise, even after uterine evacuation. Follow-up should continue for at least 6 months after the levels reach normal following evacuation. Failure to do so shows that the GTD is persistent or that GTN is present.
Follow-up should also include frequent vaginal examination is also done during this period to pick up vaginal metastases early, and to confirm that the uterus is shrinking back to normal, as expected.
Women with a molar pregnancy usually do well after evacuation. GTN may develop in up to 15 of 100 women who had complete moles, and 1 in 200 women with partial moles. GTN has a 98% cure rate following treatment.
Recurrent hydatidiform mole is very rare, and often runs in families. Certain genes have been linked to its recurrence, namely, NLRP7 and KHDC3L. Such moles are usually diploid and contain copies of DNA from both parents. The mutations are recessive in type.
Submit Comment