Intra-cytoplasmic sperm injection (ICSI) differs from conventional in vitro fertilisation (IVF) in that the embryologist selects a single sperm to be injected directly into an egg, instead of fertilisation taking place in a dish where many sperm are placed near an egg.
ICSI often is used when the male partner has fertility problems, known as male factor infertility. He may have a low sperm count, so there aren’t enough sperm to successfully fertilize an egg. His sperm may not swim well enough or strongly enough to get to the egg (motility issues) or they may not be shaped properly and can’t get through the wall of the egg (morphology issues). In other cases, the male partner may not have sperm in his ejaculate even though his testicles are producing sperm, due to blockages or abnormalities in the vas deferens, the tubes which deliver sperm from the testicles. Sperm can be extracted from his testicles and used in the lab with IVF and ICSI. ICSI may also be used if there didn’t appear to be any problems with his sperm but the previous IVF cycle did not result in fertilized eggs. ICSI makes sure the sperm gets in and increases the chance of fertilization.
You take fertility drugs to stimulate your ovaries to produce more eggs, as for IVF, and your progress will be monitored through vaginal ultrasound scans and possibly blood tests.
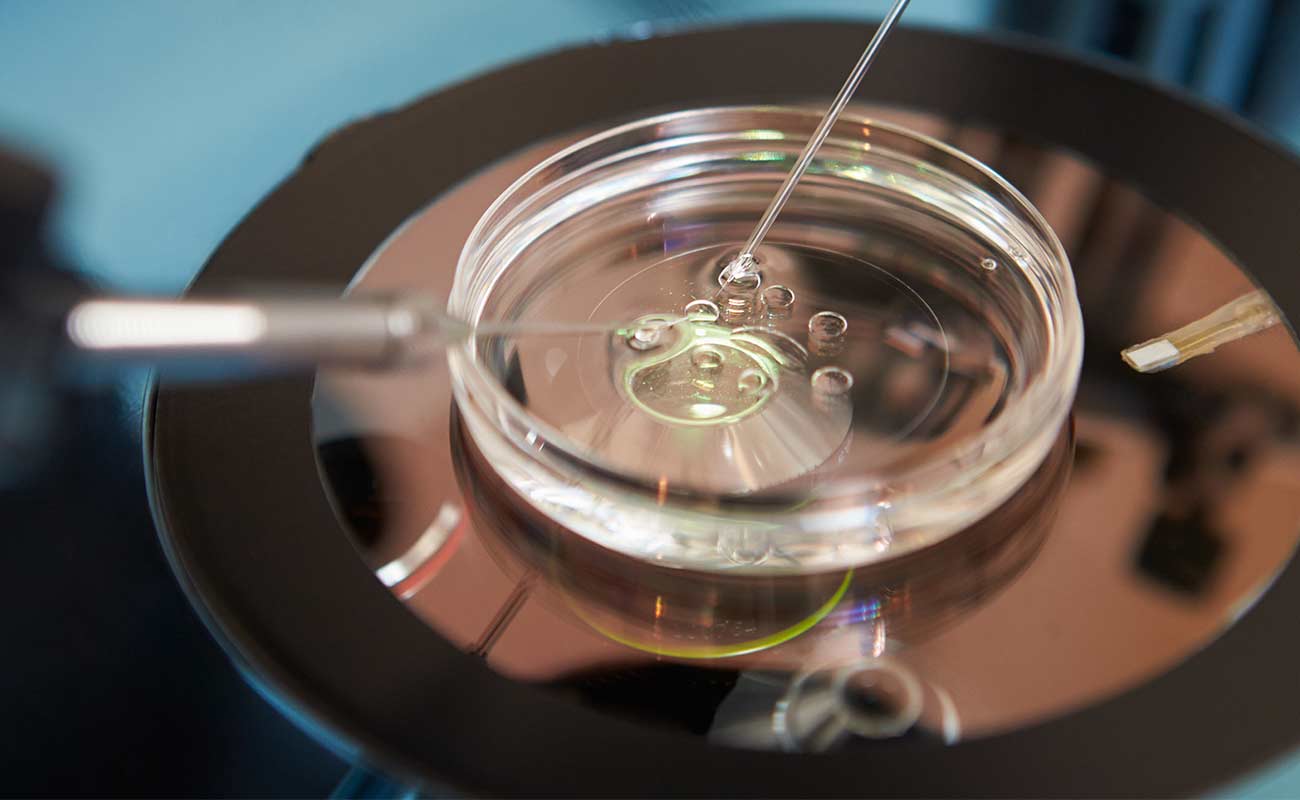
The eggs are then collected using the same procedure as IVF and each egg is injected with a single sperm from your partner or donor. The rest of the process is also the same as IVF.
You are more likely to become pregnant with twins or triplets if more than one embryo is transferred so your clinic will recommend single embryo transfer (SET) if they feel it is the best option for you. An embryologist will examine your sperm under a microscope and decide whether ICSI could increase your chances of fathering a baby.
The next step depends on whether you are able to provide sperm without a medical procedure:
Or:
A single sperm is then injected into each egg. ICSI provides the opportunity for fertilisation to happen, but it is not guaranteed to succeed.
Finally, if fertilisation does take place, the embryos will be cultured in the laboratory for up to six days and then between one and three of the best-quality embryos will be transferred to the womb.
How is ICSI carried out?
As with standard IVF treatment, fertility drugs will be needed to stimulate the ovaries to develop several mature eggs for fertilisation. Your doctor will use ultrasound, and sometimes blood tests, to monitor this stage of your treatment. When your eggs are ready for collection, you and your partner will undergo separate procedures.
Your partner will be asked to produce a sperm sample himself, by ejaculating into a cup on the same day as your eggs are collected.
If there is no sperm in his semen, or he's unable to ejaculate, it may be possible for your doctor to extract sperm from him. For that procedure, the doctor will use a fine needle to take the sperm from your partner's:

This will usually be done under a local anaesthetic, so your partner won’t feel any pain.
If these techniques don't remove enough sperm, your doctor may take a biopsy of testicular tissue, which sometimes has sperm attached. This is called testicular sperm extraction (TESE) or micro-TESE, if the surgery is carried out with a microscope. This will usually be carried out under general anaesthetic.
For practical reasons, surgical sperm extraction from the epididymis or testicle is often carried out before the treatment cycle begins. The retrieved sperm are frozen. Any discomfort felt by your partner should be mild and can be treated with painkillers.
During egg retrieval you’re likely to be sedated but conscious. The doctor will remove your eggs using a fine, hollow needle, attached to an ultrasound probe. You'll be given progesterone in the form of a pessary, or an injection of progesterone gel to help the lining of your womb prepare for egg transfer . You may feel a bit bruised and sore after egg retrieval and have some light bleeding.
Meanwhile, an embryologist isolates individual sperm in the lab and injects them into your individual eggs. A day later, the fertilised eggs will have become embryos. The procedure then follows the same steps as in IVF. Your doctor will transfer one or two embryos into your womb, through the cervix, using a fine catheter (tube) usually guided by ultrasound.
Embryos can stay in the lab for up to six days, but may be transferred two days to three days after fertilisation or at five days after fertilisation. If transferred at five days, the embryo will be at the blastocyst stage. If you're just having one embryo transferred (called Elective Single Embryo Transfer, or eSET), having a blastocyst transfer can improve your chances of a successful, healthy, single baby.
The maximum number of embryos that can be transferred to your womb is two. If you're under 40 and a suitable candidate, you may be recommended for elective single embryo transfer (eSET) in your first and second cycles. If you have one or more top-quality embryos, eSET can increase your chance of having a healthy single baby at term.
If you're 40 or over you may be offered two embryos transferred per cycle, because you have a smaller chance of conceiving with your own eggs . If the eggs are donated, again only one or two can be transferred depending on the age of the donor and the quality of the embryos.
No matter what your age, if you have a top-quality blastocyst available, this may be transferred on its own, as this is your best chance for a healthy pregnancy. Extra good-quality embryos, if there are any, may be frozen in case this cycle isn't successful or for having another baby in the future.
If all goes well, an embryo will attach to the wall of your womb and continue to grow to become your baby. After about two weeks, you will be able to take a pregnancy test.
How long does ICSI treatment last?
One cycle of ICSI takes between four weeks and six weeks to complete. You and your partner can expect to spend a half-day at the clinic for the egg and sperm retrieval procedures. You will usually be asked to go back between two days and five days later for the embryo transfer procedure.
If you’re under 40, you should be offered up to three full cycles of IVF with or without ICSI. If you’re aged between 40 and 42 years old, you’ve never had IVF before and you have no sign of low egg numbers, you should be offered one full cycle after full discussion of the implications of IVF and pregnancy at this age.

Fertilization rates for ICSI: Most IVF programs see that about 70-85% of eggs injected using ICSI become fertilized. We call this the fertilization rate, which is different from the pregnancy success rate.
Pregnancy success rates for in vitro fertilization procedures with ICSI have been shown in some studies to be higher than for IVF without ICSI. This is because in many of the cases needing ICSI the female is relatively young and fertile (good egg quantity and quality) as compared to some of the women having IVF for other reasons.
In other words, the average egg quantity and quality tends to be better in ICSI cases (male factor cases) because it is less likely that there is a problem with the eggs - as compared to cases with unexplained infertility. Some unexplained cases have reduced egg quantity and/or quality - which lowers the chances for a successful IVF outcome.
IVF with ICSI success rates vary according to the specifics of the individual case, the ICSI technique used, the skill of the individual performing the procedure, the overall quality of the laboratory, the quality of the eggs, and the embryo transfer skills of the infertility specialist physician.
Sometimes IVF with ICSI is done for "egg factor" cases - low ovarian reserve situations. This is when there is either a low number, or low "quality"of eggs (or both). In such cases, ICSI fertilization and pregnancy success rates tend to be lower.
In some cases, assisted hatching is done on the embryos prior to transfer, in order to maximize chances for pregnancy.
The good news is, ICSI’s effect on birth defects is very slight. A normal pregnancy without assisted reproductive technology (ART) has a 1.5 percent to 3 percent chance of birth defects. ICSI treatment causes a very slightly increased chance, and birth defects are extremely rare. Long-term studies have found some specific risks of birth defects, which may be due to lower quality sperm, including sex chromosome abnormalities, defects in the urinary system or genitals, and other rare syndromes such as Angelman syndrome, hypospadias, and sex chromosome abnormailities. But, again, the chance of this happening appears to be very low.
The American Society for Reproductive Medicine (ASRM) estimates the average price of an IVF cycle in the U.S. at $12,400. This does not include the cost of fertility medications and doesn’t include other procedures such as ICSI and PGD (preimplantation genetic diagnosis). The cost of ICSI is an additional $1,500 to $2,000.
The cost of this procedure is much lower in Iran. It is estimated that the cost of performing ICSI in Iran is 0.25 to 0.35 of what the patient will be charged in the USA.
winfertility, hfea.gov.uk, advancedfertility
Submit Comment