Glaucoma is a chronic, progressive deterioration of the optic nerve (the bundle of nerve fibers at the back of the eye that carry visual messages from the retina to the brain). It is usually caused by or worsened by pressure inside the eye (intraocular pressure, or IOP) that is too high for the continued health of the nerve. The only proven treatment of glaucoma is lowering of IOP in order to prevent or to slow down the damage to the optic nerve. Glaucoma treatment usually begins with medications or laser techniques, but when these have failed or are not tolerated, your ophthalmologist may suggest surgical procedures. The delicate, microscopic incisional methods include trabeculectomy with or without ExPRESS microshunt implantation, tube shunt (glaucoma drainage device) implantation, and cyclophotocoagulation. There are also newer procedures called MIGS, or minimally invasive glaucoma surgery. Each has its own special uses, advantages and disadvantages. In this article we will discuss the risks and benefits of glaucoma surgery.
The signs and symptoms of glaucoma vary depending on the type and stage of your condition. For example:
Open-angle glaucoma
Acute angle-closure glaucoma
If left untreated, glaucoma will eventually cause blindness. Even with treatment, about 15 percent of people with glaucoma become blind in at least one eye within 20 years.
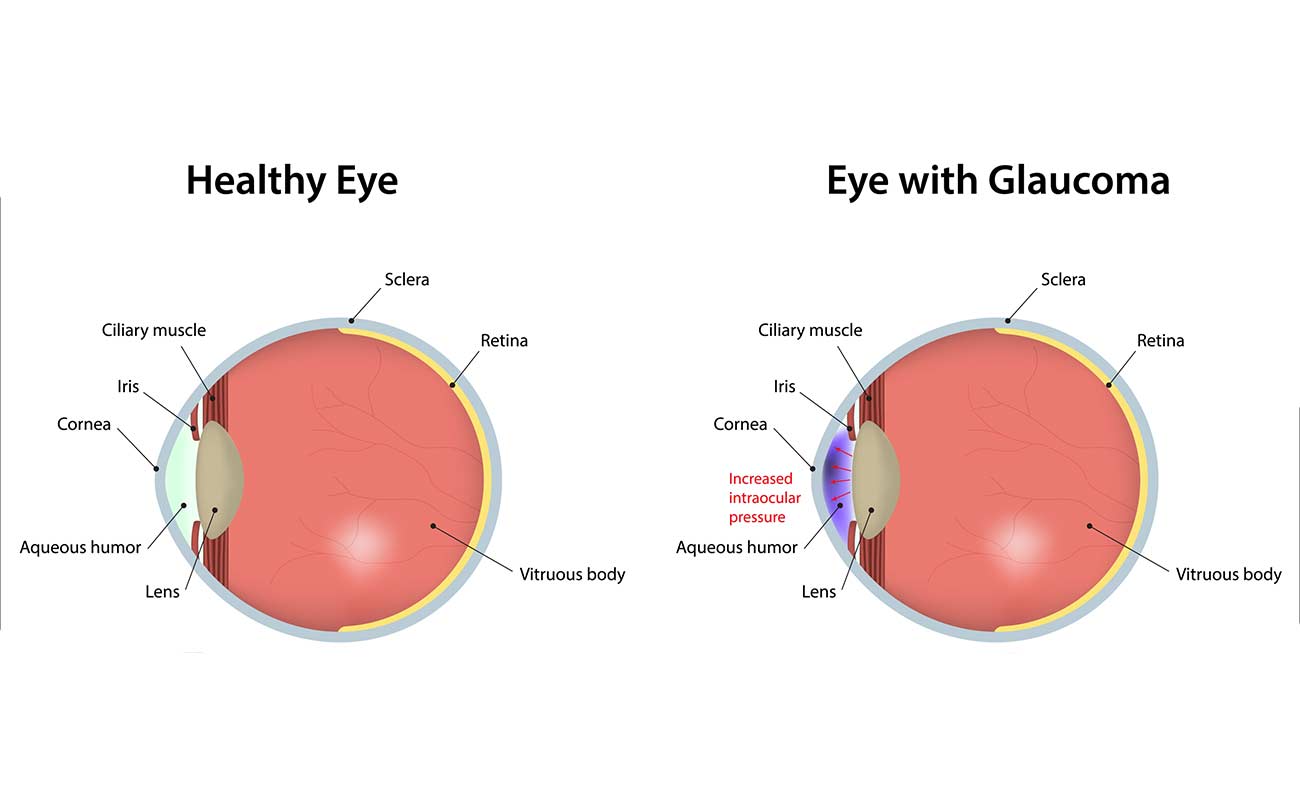
The cause of glaucoma generally is a failure of the eye to maintain an appropriate balance between the amount of internal (intraocular) fluid produced and the amount that drains away.
Underlying reasons for this imbalance usually relate to the type of glaucoma you have.
Just as a basketball or football requires air pressure to maintain its shape, the eyeball needs internal fluid pressure to retain its globe-like shape and ability to see.
But when something affects the ability of internal eye structures to regulate intraocular pressure (IOP), eye pressure can rise to dangerously high levels — causing glaucoma.
Unlike a ball or balloon, the eye can't relieve pressure by springing a leak and "deflating" when pressure is too high. Instead, high eye pressure just keeps building and pushing against the optic nerve until nerve fibers are permanently damaged and vision is lost.
While high IOP often is associated with glaucoma, this eye disease also can occur when internal eye pressure is normal (normal-tension glaucoma). People with this condition have highly pressure-sensitive optic nerves that are susceptible to irreversible damage from what ordinarily would be considered "normal" IOP.
Conversely, certain people with elevated intraocular pressure known as ocular hypertension may never develop glaucoma.
Most conventional methods of screening for glaucoma involve testing eyes for the presence of high IOP. But because glaucoma can occur even without high IOP, direct examination of the optic nerve and visual field testing are essential in making (or ruling out) the diagnosis of glaucoma.
Though the exact cause of normal-tension glaucoma is unknown, many researchers believe decreased blood flow to the optic nerve may be a factor. This could be caused by narrowing of blood vessels that nourish the optic nerve or constrictions of these vessels (vasospasms).
Some studies also indicate that poor blood flow within the eye is associated with blind spots (scotomas) that develop within the visual field, similar to those that occur in glaucoma.*
An intriguing study reported in August 2007 indicates a potential common cause of both glaucoma and Alzheimer's, which creates brain lesions and accompanying memory loss.

Researchers in the UK who conducted the study found that buildup of a protein known as beta-amyloid in the eye's retina and in brain tissue appears to be associated with development of both glaucoma and Alzheimer's.
However, abnormal accumulation of beta-amyloid proteins does not mean that someone with Alzheimer's will have glaucoma or vice versa. Researchers said similarities between certain eye and brain tissue could explain why the buildup of beta-amyloid proteins can affect both the eye and the brain
The only sure way to diagnose glaucoma is with a complete eye exam. A glaucoma screening that only checks eye pressure is not enough to find glaucoma.
During a glaucoma exam, your ophthalmologist will:
Medication
Glaucoma is usually controlled with eyedrop medicine. Used every day, these eye drops lower eye pressure. Some do this by reducing the amount of aqueous fluid the eye makes. Others reduce pressure by helping fluid flow better through the drainage angle.

Glaucoma medications can help you keep your vision, but they may also produce side effects. Some eye drops may cause:
All medications can have side effects. Some drugs can cause problems when taken with other medications. It is important to give your doctor a list of every medicine you take regularly. Be sure to talk with your ophthalmologist if you think you may have side effects from glaucoma medicine.
Never change or stop taking your glaucoma medications without talking to your ophthalmologist. If you are about to run out of your medication, ask your ophthalmologist if you should have your prescription refilled.
Laser surgery
There are two main types of laser surgery to treat glaucoma. They help aqueous drain from the eye. These procedures are usually done in the ophthalmologist’s office or an outpatient surgery center.
Some glaucoma surgery is done in an operating room. It creates a new drainage channel for the aqueous humor to leave the eye.

Sources: mayoclinic.org, glaucoma.org, allaboutvision.com, aao.org, glaucomafoundation.org.
Submit Comment