A brain abscess forms when fungi, viruses, or bacteria reach your brain through a wound in your head or an infection somewhere else in your body. According to the Children’s Hospital of Wisconsin, infections from other parts of the body account for between 20 and 50 percent of all brain abscess cases. Heart and lung infections are among the most common causes of brain abscesses. However, brain abscesses can also begin from an ear or sinus infection, or even an abscessed tooth.
See your doctor right away if you think you may have a brain abscess. You’ll need the appropriate treatment to prevent any brain damage from the swelling.
Symptoms may develop slowly, over a period of 2 weeks, or they may develop suddenly. They may include:
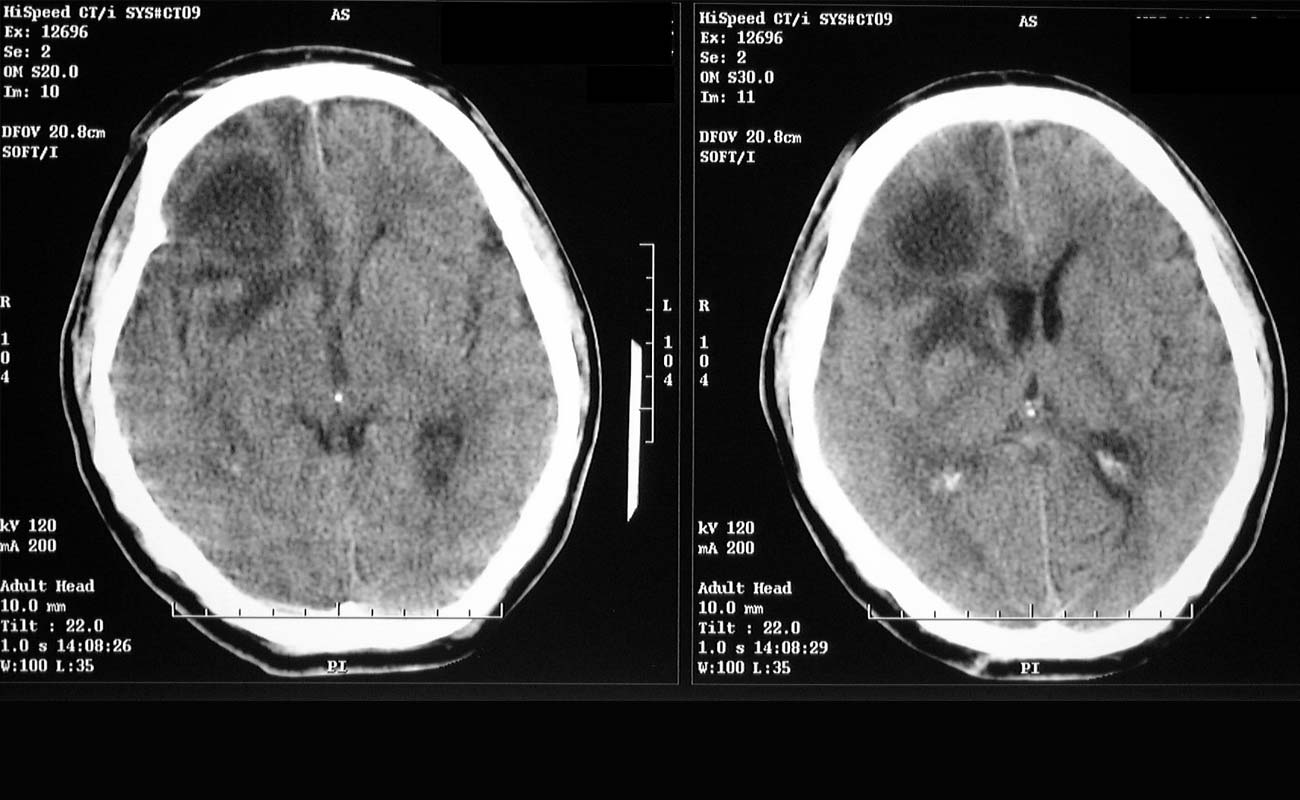
When symptoms suggest an abscess, contrast-enhanced MRI or, if unavailable, contrast-enhanced CT is done. A fully developed abscess appears as an edematous mass with ring enhancement, which may be difficult to distinguish from a tumor or occasionally infarction; CT-guided aspiration, culture, surgical excision, or a combination may be necessary.
Culturing pus aspirated from the abscess can make targeted antibiotic therapy of the abscess possible. However, antibiotics should not be withheld until culture results are available.
Lumbar puncture is not done because it may precipitate transtentorial herniation and because CSF findings are nonspecific
The most common causes of a brain abscess, also known as a cerebral abscess, are bacteria or fungi infecting part of the brain. Parasites may also cause brain abscesses. The most common bacteria recovered from cultures are Streptococcus cocci.
When the bacteria, fungi or parasite infect part of the brain, inflammation (swelling) occurs. Infected brain cells, immune cells (white blood cells), live and dead organisms (fungi, bacteria, parasites) accumulate, a membrane forms around the area, creating a mass.
Our immune system creates the membrane to isolate the infection; however, sometimes our defense mechanism does more harm than good.
If the mass (abscess) swells it places increasing pressure on brain tissue. The skull is not flexible; it does not expand. The mass can block blood vessels to the brain, resulting in the possible destruction of delicate brain tissue.
Put simply:
The blood-brain barrier
Brain infections are fairly uncommon for several reasons, one of which is the blood-brain barrier. This is a protective network of blood vessels and cells that filters out impurities from blood flowing to the brain.
Sometimes an infection can get through the blood-brain barrier and infect the brain. Experts are not entirely sure why this happens. The infection enters the brain from three main routes:
The location of the abscess may help the doctor identify where the primary lesion is (where the original infection is):
Fungi and parasites tend to cause brain abscesses in patients with weakened immune systems. Poliovirus, Taoxoplasma gondii, and Cryptococcus neoformans most frequently cause brain abscesses in patients with AIDS.

Before the abscess has become encapsulated and localized, antimicrobial therapy, accompanied by measures to control increasing intracranial pressure, is essential. Once an abscess has formed, surgical excision or drainage combined with prolonged antibiotics (usually 4-8 wk) remains the treatment of choice. Some neurosurgeons advocate complete evacuation of the abscess, while others advocate repeated aspirations as indicated.
The first step is to verify the presence, size, and number of abscesses using contrast CT scanning or MRI.
Emergent surgery should be performed if a single abscess is present. Abscesses larger than 2.5 cm are excised or aspirated, while those smaller than 2.5 cm or which are at the cerebritis stage are aspirated for diagnostic purposes only.
In cases of multiple abscesses or in abscesses in essential brain areas, repeated aspirations are preferred to complete excision. High-dose antibiotics for an extended period may be an alternative approach in this group of patients.
An early effort at making a microbiologic diagnosis is important in planning appropriate antimicrobial therapy. The introduction of CT-guided needle aspiration may provide this important information. Frequent scanning, at least once per week, is essential in monitoring treatment response. Although surgical intervention remains an essential treatment, selected patients may respond to antibiotics alone.
Corticosteroid use is controversial. Steroids can retard the encapsulation process, increase necrosis, reduce antibiotic penetration into the abscess, increase the risk of ventricular rupture, and alter the appearance on CT scans because of contrast reduction. Steroid therapy can also produce a rebound effect when discontinued. Corticosteroids are used when a significant mass effect is visible on imaging and the patient’s mental status is depressed. When used to reduce cerebral edema, therapy should be of short duration. The appropriate dosage, the proper timing, and any effect of steroid therapy on the course of the disease are unknown.
Numerous factors should be considered when trying to decide the appropriate approach to therapy. Abscesses smaller than 2.5 cm generally respond to antimicrobial therapy, while abscesses larger than 2.5 cm have failed to respond to such treatment.
Knowledge of the etiologic agent or agents by recovery from blood, CSF, abscess, or other normally sterile sites is essential because it allows for the most appropriate selection of antimicrobial agents.
The duration of the symptoms before diagnosis is an important factor. Bacterial abscess in the brain is preceded by infarction and cerebritis. Antibiotic therapy during the early stage, when no evidence of an expanding mass lesion exists, may prevent the progress from cerebritis to abscess.
Patients who have symptoms for less than a week have a more favorable response to medical therapy than patients with symptoms persisting longer than 1 week.
Patients treated with medical therapy alone usually demonstrate clinical improvement before significant changes in the CT scan are observed.
CT scanning and MRI should eventually show a decrease in the size of the lesion, a decrease in accompanying edema, and a lessening of the enhancement ring. Improvement on CT scans is generally observed within 1-4 weeks (average, 2.5 wk) and complete resolution in 1-11 months (average, 3.5 mo).
Antimicrobial treatment for a brain abscess is generally long (6-8 wk) because of the prolonged time needed for brain tissue to repair and close abscess space. The United Kingdom treatment guidelines advocate 4-6 weeks if the abscess has been drained or removed and 6-8 weeks if drainage occurred. The antimicrobial course is through an intravenous route. There is no evidence that transition to oral therapy is appropriate. Furthermore, the concentrations of most oral antibiotics (except for metronidazole, rifampin, linezolid, and trimethoprim-sulfamethoxazole) in the abscess cavity would be inadequate to eradicate the pathogens.
The duration of therapy can be adjusted according to the patient’s condition, causative organism(s), number of abscesses and their size, and response to treatment. A shorter course (4-6 wk) may suffice for cerebritis and in patients who underwent surgical drainage. [37] A long course (>6 wk) is required for necrotic and/or encapsulated abscess with tissue necrosis, multiloculated abscess, abscesses in vital intracranial locations (ie, brain steam), and in immunocompromise.
The length of therapy is guided by continuous assessment of the clinical course and followup imaging studies. The antimicrobial therapy is continued until a clinical response occurs and CT or MRI findings show resolution. However, because the abscess site may show persistent enhancement for several months. This finding alone is not an indication to continue antimicrobial therapy or for surgical drainage.
Because of the difficulty involved in the penetration of various antimicrobial agents through the blood-brain barrier, the choice of antibiotics is restricted, and maximal doses are often necessary.
Initial empiric antimicrobial therapy should be based on the expected etiologic agents according to the likely predisposing conditions, the primary infection source, and the presumed pathogenesis of abscess formation. When abscess specimens are available, staining of the material can help guide selection of therapy. Whenever proper cultures are taken and organisms are isolated and their susceptibility is determined, the initial empiric therapy can be adjusted to specifically treat the isolated bacteria.
Coverage for streptococci can be attained by a high dose of penicillin G or a third-generation cephalosporin (eg, cefotaxime, ceftriaxone). Metronidazole is included to cover penicillin-resistant anaerobes (ie, gram-negative bacilli). This choice is appropriate for the treatment of an abscess of oral, otogenic, or sinus origin.
When S aureus is suspected (a hematogenic origin, or following neurosurgery or penetrating trauma), vancomycin (effective against methicillin resistance S aureus) is administered. Metronidazole may be added to cover anaerobic bacteria.
Cefepime or ceftazidime is administered to treat gram negative aerobic bacteria Pseudomonas aeruginosa infection.
Patients with HIV infection may require therapy for toxoplasmosis.
Specific antibiotics
Penicillin penetrates well into the abscess cavity and is active against non–beta–lactamase-producing anaerobes and aerobic organisms. However, the emergence of beta–lactamase-producing organisms limits it use.
Chloramphenicol penetrates well into the intracranial space and is also active against Haemophilus species, S pneumoniae, and most obligate anaerobes. Its use has been curtailed dramatically in most US centers because of the availability of other equally efficacious and less toxic antimicrobial combinations (ie, cefotaxime plus metronidazole).
Metronidazole penetrates well into the CNS and is not affected by concomitant corticosteroid therapy. However, it is only active against strict anaerobic bacteria, and its activity against anaerobic gram-positive anaerobes may be suboptimal.
Third-generation cephalosporins (eg, cefotaxime, ceftriaxone) generally provide adequate therapy for aerobic gram-negative organisms as well as microaerophilic and aerobic streptococci. If pseudomonads are isolated or anticipated, the parenteral cephalosporin of choice is a forth generation cephalosporin (ceftazidime or cefepime).
Aminoglycosides do not penetrate well into the CNS and are relatively less active because of the anaerobic conditions and the acidic contents of the abscess.
Beta-lactamase–resistant penicillins (eg, oxacillin, methicillin, nafcillin) provide good coverage against methicillin-sensitive S aureus (MSSA). However, their penetration into the CNS is less than penicillin, and the addition of rifampin has been shown to be of benefit in staphylococcal meningitis. Because of the risk of methicillin-resistant S aureus (MRSA) infection they should only be administered to treat culture proved MSSA.
Vancomycin is most effective against MRSA and Staphylococcus epidermidis as well as aerobic and anaerobic streptococci and Clostridium species.
Antimicrobial that are alternatives to vancomycin include linezolid (600 mg IV or PO bid), trimethoprim-sulfamethoxazole (5 mg/kg q8-12h), and daptomycin (6 mg/kg IV qd). Limited data regarding their use in brain abscess are available. However, they may be considered in instances in which vancomycin is ineffective or can not be used.
With the exception of the Bacteroides fragilis group and some strains of Prevotella species, Porphyromonas species, and Fusobacterium species, most of the anaerobic pathogens isolated are sensitive to penicillin. Because these penicillin-resistant anaerobic organisms predominate in brain abscesses, empiric therapy should include agents effective against them that can also penetrate the blood-brain barrier. These include metronidazole, chloramphenicol, ticarcillin plus clavulanic acid, imipenem, and meropenem.
Caution should be used in administering carbapenems and beta-lactamases in general, because high doses of these agents may be associated with seizure activity. Imipenem has been associated with an increased risk of seizures in patients with brain abscess. Although fluoroquinolones have good penetration into the CNS, data are limited regarding their use in treating brain abscesses.
Therapy with penicillin should be added to metronidazole to cover aerobic and microaerophilic streptococci.
The administration of beta-lactamase–resistant penicillin or vancomycin (if methicillin-resistant staphylococci are isolated) for the treatment of S aureus is generally recommended.
Amphotericin B is administered for Candida, Cryptococcus, and Mucorales infections; voriconazole for Aspergillus and P boydii infections.
T gondii infection is treated with pyrimethamine and sulfadiazine.
Injection of antibiotics into the abscess cavity was advocated in the past in an effort to sterilize the area before operation. However, many antimicrobials penetrate brain abscess cavities fairly well, and instillation of antibiotics into the abscess after drainage is not needed.
Surgical drainage provides the most optimal therapy. The procedures used are aspiration through a bur hole and complete excision after craniotomy. These procedures are also diagnostic and provide material that can guide antimicrobial therapy.
Needle aspiration is the preferred and the most commonly used procedure and is often performed using a stereotactic procedure with the guidance of ultrasound or CT scanning. [36] For optimal results, this is usually performed prior to the initiation of antibiotic therapy. It is repeated if the patient fails to respond to therapy. Aspiration is especially preferred if the speech, motor or sensory cortex area are involved or the patient is comatose. Craniotomy is generally performed in patients with multiloculated abscesses and in those whose conditions fail to resolve. [41]
Ventricular drainage combined with administration of intravenous and/or intrathecal antimicrobials is used to treat brain abscesses that rupture into the ventricles.
If not recognized early, both subdural empyema and brain abscess can be fatal. Emergent surgery is needed if neurologic signs related to a mass lesion progress.
Antibiotics have improved the outlook.
Management of subdural empyema requires prompt surgical evacuation of the infected site and antimicrobial therapy.
Failure to perform surgical drainage can lead to a higher mortality rate.
Although proper selection of antimicrobial therapy is most important in the management of intracranial infections, surgical drainage may be required. Optimal therapy of fungal brain abscess generally requires both medical and surgical approach.
A delay in surgical drainage and decompression can be associated with high morbidity and mortality.
Recent studies illustrate that brain abscess in the early phase of cerebritis may respond to antimicrobial therapy without surgical drainage.
Surgical drainage may be necessary in many patients to ensure adequate therapy and complete resolution of infection.
Patients who do not meet the criteria for medical therapy alone require surgery. Currently, 2 surgical approaches are available: stereotactic-guided aspiration and excision. Needle aspiration is generally preferred to surgical excision because it results in fewer sequelae. Drainage may be delayed or avoided if the infection is at the cerebritis stage or the lesion is at a vital or inaccessible region.
The risk of repeating aspiration is that the procedure may cause bleeding.
Excision is clearly indicated in posterior fossa or multiloculated abscesses, those caused by unencapsulated lesions due to fungal or helminthic infection, those associated with traumatic brain injury (to remove foreign material), and those that reaccumulate following repeated aspirations. Excision is also indicated even after initial aspiration or drainage in patients with depressed sensorium, increased intracranial pressure, no clinical improvement within 7 days, and/or a progressively growing abscess.
Submit Comment