The pancreas is a large gland located behind the abdominal and beside the small intestine. There are two main functions for pancreas:
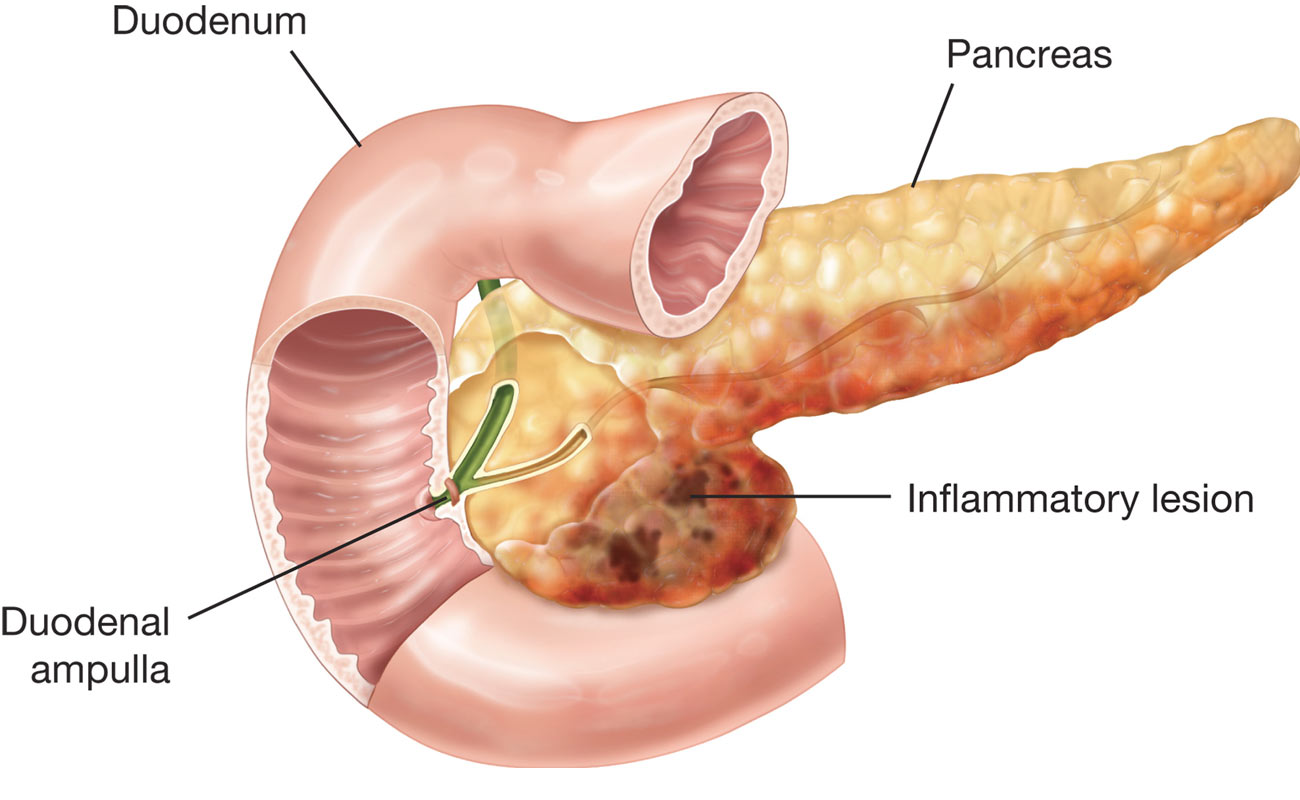
Pancreatitis is a disorder of having an inflamed pancreas. Damage to pancreas occurs when the digestive enzymes get triggered before they are send into the small intestine. At this time, the enzymes start attacking the pancreas.
Two forms of pancreatitis are acute and chronic.
Acute pancreatitis as quick swelling continues for a short period of time. It might be trivial or mild discomfort or a serious, mortal disease. Most of those with acute pancreatitis fully recover after receiving the proper treatment. In serious cases, acute pancreatitis could lead to bleeding into the gland, severe damage in tissues, contagion, and creation of cyst. Serious pancreatitis could damage the other parts of the body such as the heart, kidneys, and lungs.
Depanding on the type of pancreatitis, different symptoms may be observed.
Some of the signs and symptoms of acute pancreatitis are as follows:
Also, some of the signs and symptoms of chronic pancreatitis are:
If you are experiencing stomach pain, instantly make an appointment with a doctor. If the pain in your stomach is severe so that you can't sit or have a comfortable position, immediately look out for some medical support.

Trypsin as a digestive enzyme which is secreted in the pancreas in the form of inactive enzyme; it is known that alcohol misuse may activate trypsin before it is out of the pancreas. It is believed that ethanol molecules affecting the pancreas cells and whereby causing them to activate trypsin constantly.
Instances of bacterial infections that may lead to acute pancreatitis are Salmonellosis (kind of food poisoning initiated by Salmonella) or Legionnaires' disorder (an infection caused by Legionella pneumophila found in water-storage tanks and plumbing shower heads. Acute pancreatitis may also be initiated by some specific viruses, including hepatitis B, mumps, coxsackievirus, cytomegalovirus, and varicella-zoster virus.
Gallstones are those small, stone-like formations that grow in the gallbladder mostly as result of existence of too much cholesterol in the bile. Occasionally, when the gallstones start getting out of the bile ducts and going into the intestines get stuck. This obstruction may as well prevent the pancreas from the enzymes in the intestines. At those occasions when acute pancreatitis is connected to gallstones, physicians usually recommend elective removal of the gallbladder while the patient is still in the hospital.

Pancreatitis may create serious complications for the patient, some of which are:
Treating mild pancreatitis typically includes short-term hospitalization where analgesics are recommended for pain relief and the patent fasts to rest the pancreas. Typically, regular eating could be start again after 2 to 3 days without any additional treatment.

Patients with mild or serious pancreatitis are required to be admitted to hospital. These patients must originally avid eating and drinking, since food and drink rouse the pancreas. In moderate pancreatitis, avoiding food and drink could continue for a few days or several weeks. Symptoms like pain and unsettled stomach could be controlled through intravenously injected medications. Also, intravenous fluids might be prescribe. Those patient with serious acute pancreatitis are hospitalized in an intensive care unit because their vital signs (pulse, blood pressure, and breath rate) as well as urine production should be carefully monitored. Blood samples should be repeatedly taken because the different components of the blood have to be monitored. These component include sugar (glucose) levels, electrolyte levels, hematocrit, white blood cell count, and amylase and lipase levels. Nasogastric tube (a tupe inserted through the nose into the abdominal) might be introduced to take a way fluid and air. It is mostely used if unsettled stomach and vomiting continue and gastrointestinal ileus exists. Nutrition is also given intravenously or orally.
Doctors may also prescribe some medications including histamine-2 (H2) blockers or a proton pump inhibitors, to decrease or prevent the creation of stomach acid.
For those who have with low blood pressure or are in shock, blood volume is maintained with intravenous fluids, also heart function is carefully monitored. Some ill people need supplemental oxygen which is provided through ventilator.
An infection is treated with the help of antibiotics. However, surgical removal of infected and dead tissues might be crucial.
A pseudocyst should be drained or taken away through surgery or catheter (all has to do with the location of the pseudocyst). Catheter may be inserted through the skin or by endoscopic procedure, through which a small tube is passed through the mouth into the abdominal or intestine. The catheter provides the drain of the pseudocyst for many weeks.
Surgeon perform surgery almost immediately if pancreatitis has occurred due to a severe blunt or sharp damage or unrestrained biliary sepsis.
If gallstones is the cause of the acute pancreatitis, treatments will be prescribed based on the severity of the condition. If the pancreatitis is mediocre, gallbladder removal is typically put off till the severity of symptoms gets lower. If the pancreatitis caused by gallstones is thought to be Severe, endoscopic retrograde cholangiopancreatography will usually be implemented. Although most of the people (higher than 80 percent) with gallstone pancreatitis pass the stone naturally, for those who show no improvement over the first 24 hours of hospitalization, ERCP with stone removal is usually required.
Submit Comment