Achalasia is a rare disease of the muscle of the esophagus (swallowing tube). The term achalasia means "failure to relax" and refers to the inability of the lower esophageal sphincter (a ring of muscle situated between the lower esophagus and the stomach) to open and let food pass into the stomach. As a result, people with achalasia have difficulty swallowing food. In addition to the failure to relax, achalasia is associated with abnormalities of esophageal peristalsis (usually complete absence of peristalsis), the coordinated muscular activity of the body of the esophagus (which comprises 90% of the esophagus) that transports food from the throat to the stomach.
How does the normal esophagus function?
The esophagus has three functional parts. The uppermost part is the upper esophageal sphincter, a specialized ring of muscle that forms the upper end of the tubular esophagus and separates the esophagus from the throat. The upper sphincter remains closed most of the time to prevent food in the main part of the esophagus from backing up into the throat. The main part of the esophagus is referred to as the body of the esophagus, a long, muscular tube approximately 20 cm (8 in) in length. The third functional part of the esophagus is the lower esophageal sphincter, a ring of specialized esophageal muscle at the junction of the esophagus with the stomach. Like the upper sphincter, the lower sphincter remains closed most of the time to prevent food and acid from backing up into the body of the esophagus from the stomach.
The upper sphincter relaxes with swallowing to allow food and saliva to pass from the throat into the esophageal body. The muscle in the upper esophagus just below the upper sphincter then contracts, squeezing food and saliva further down into the esophageal body. The ring-like contraction of the muscle progresses down the body of the esophagus, propelling the food and saliva towards the stomach. (The progression of the muscular contraction through the esophageal body is referred to as a peristaltic wave.). By the time the peristaltic wave reaches the lower sphincter, the sphincter has opened, and the food passes into the stomach.
How is esophageal function abnormal in achalasia?
In achalasia there is an inability of the lower sphincter to relax and open to let food pass into the stomach. In at least half of the patients, the lower sphincter resting pressure (the pressure in the lower sphincter when the patient is not swallowing) also is abnormally high. In addition to the abnormalities of the lower sphincter, the muscle of the lower half to two-thirds of the body of the esophagus does not contract normally, that is, peristaltic waves do not occur, and, therefore, food and saliva are not propelled down the esophagus and into the stomach. A few patients with achalasia have high-pressure waves in the lower esophageal body following swallows, but these high-pressure waves are not effective in pushing food into the stomach. These patients are referred to as having "vigorous" achalasia. These abnormalities of the lower sphincter and esophageal body are responsible for food sticking in the esophagus.

People with achalasia will often have trouble swallowing or feel like food is stuck in their esophagus. This is also known as dysphagia. This symptom can cause coughing and raises the risk of aspiration, or inhaling or choking on food. Other symptoms include:
You might also have regurgitation or backflow. However, these can be symptoms of other gastrointestinal conditions such as acid reflux.

In achalasia, nerve cells in the esophagus (the tube that carries food from the mouth to the stomach) degenerate for reasons that are not known. The loss of nerve cells in the esophagus causes two major problems that interfere with swallowing:
●The muscles that line the esophagus do not contract normally, so that swallowed food is not propelled through the esophagus and into the stomach properly.
●The lower esophageal sphincter (LES), a band of muscle that encircles the lower portion of the esophagus, does not function correctly.
Normally, the LES relaxes when we swallow to allow swallowed food to enter the stomach. When the food has moved through the esophagus into the stomach, the LES muscle contracts to squeeze the end of the esophagus closed, thus preventing the stomach contents from flowing backwards (refluxing) into the esophagus.
In people with achalasia, the LES fails to relax normally with swallowing. Instead, the LES muscle continues to squeeze the end of the esophagus, creating a barrier that prevents food and liquids from passing into the stomach. Over time, the esophagus above the persistently contracted LES dilates, and large volumes of food and saliva can accumulate in the dilated esophagus.
If your GP thinks you have achalasia, you will be referred to hospital to have some diagnostic tests performed.
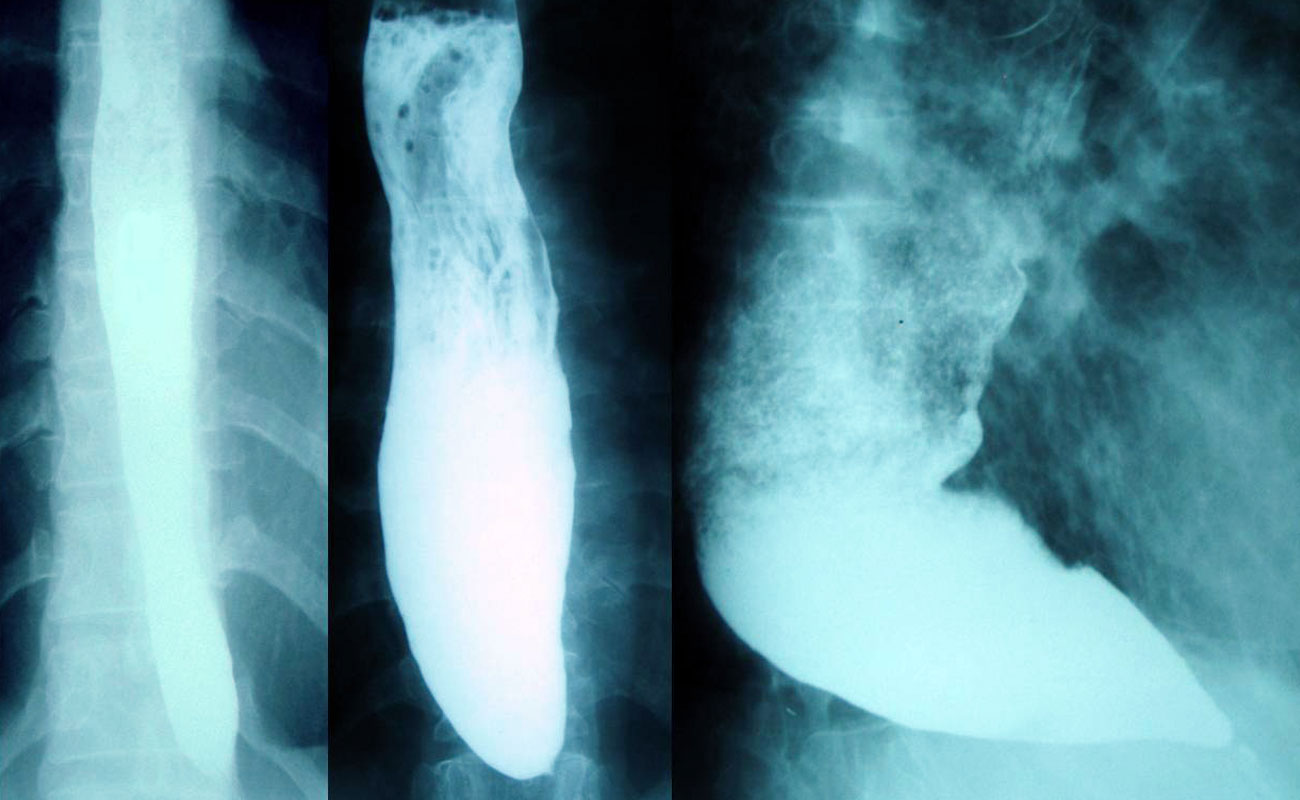
A barium swallow involves drinking a white liquid containing the chemical barium, which allows the gullet to be seen and videoed on an X-ray.
In achalasia, the exit at the lower end of your gullet never opens properly, which causes a delay in barium passing into your stomach.
An ordinary chest X-ray may show a wide gullet.
A flexible instrument called an endoscope is passed down your throat to allow the doctor to look directly at the lining of your gullet and stomach. Trapped food will be visible.
The endoscope can be passed through the tight muscle at the bottom of your gullet and into your stomach to check there is no other disorder of the stomach.
Read more about having an endoscopy.
Manometry measures pressure waves in your gullet. A small plastic tube is passed into your gullet through your mouth or nose and the pressure at different points in your gullet is measured.
In achalasia, there are usually weak or absent contractions of the gullet and sustained high pressure in the muscle at the lower end of the gullet. The high pressure means the muscle does not relax in response to swallowing, causing symptoms of achalasia.

If left untreated, achalasia can be debilitating. People with the condition experience considerable weight loss that can result in malnutrition. Lung infections and pneumonia due to aspiration of food can result, particularly in the elderly.
There are several successful treatments available for achalasia, including:
Today, achalasia can be treated successfully by laparoscopy. Using five small incisions, a Heller myotomy can be accomplished (called laparoscopic Heller myotomy). It has been shown that the addition of a partial fundoplication (Dor) minimizes reflux and protects the esophagus from damaging gastroesophageal reflux. This operation usually requires one day of hospital stay and recovery is typically accelerated when compared to conventional surgery.
Your health care team will discuss the possible risks and benefits of each treatment option with you.
It must be remembered that treatment of achalasia does not fix the esophagus, it only attempts to improve esophageal emptying. This, however, is at the risk of allowing the stomach to empty it contents into the esophagus (reflux).
Regardless of the therapy, long-term follow up is necessary to assure that the esophagus can be preserved as a passive conduit. This requires adequate esophageal emptying after the treatment of choice and prevention of gastroesophageal reflux. The obstructed esophagus or one that is subjected to reflux will dilate and expand and may eventually need to be replaced.
Since the underlying cause for achalasia is unknown, it is not possible to restore the function of the esophagus. Most patients will have some residual symptoms after successful treatment but should be able to eat almost normally.
Cancer risk
If the gullet contains a large amount of food that does not pass into the stomach in the normal way, the risk of cancer of the oesophagus (gullet) is slightly increased.
The increased risk is likely to be most significant in long-term untreated achalasia. It's therefore important to get appropriate treatment for achalasia straight away, even if your symptoms are not bothering you.
According to Cancer Research UK, compared with the general population:
However, cancer of the oesophagus is very uncommon and although your risk is slightly increased, it remains highly unlikely.
· Golden, AK. Decision Support System. Mayo Clinic, Rochester, Minn. Feb. 18, 2015.
· Spechler SJ. Clinical manifestations and diagnosis of achalasia. http://www.uptodate.com/home. Accessed Feb. 18, 2015.
· Spechler SJ. Overview of the treatment of achalasia. http://www.uptodate.com/home. Accessed Feb. 18, 2015.
Submit Comment