The decision to continue your pregnancy or to end it is very personal.Each year, nearly 1.2 million American women have an abortion to end a pregnancy.

The most common reasons women consider abortion are:
When discussing abortion for medical reasons, we are usually talking about birth defects or chromosomal abnormalities in the baby. In some cases, a pregnancy can place the mother's life in danger. In that case, a termination of pregnancy would also have a medical reason. A third situation in which abortion comes up is a higher order multiple pregnancy. A pregnancy of triplets or beyond places a serious strain on the mother's body, but a pregnancy of so many fetuses also puts the fetuses themselves at risk. Finally, "abortion" can be carried out after a fetus has passed away inside the mother's uterus. This is called a dilation and curettage or dilation and evacuation (D&C or D&E, different procedures with the same aim) and they are not carried out beyond the second trimester of pregnancy.

Your doctor will ask about your medical history and examine you. Even if you used a home pregnancy test, another pregnancy test often is needed to confirm that you are pregnant. In some cases, you will need an ultrasound to determine how many weeks into the pregnancy you are and the size of the fetus, and to make sure the pregnancy is not ectopic.
An ectopic pregnancy is one that is growing outside of the uterus. An ectopic pregnancy usually occurs in the tube that carries the egg from the ovary to the uterus (Fallopian tube) and is commonly called a tubal pregnancy.
A blood test will determine your blood type and whether you are Rh positive or negative. The Rh protein is made by the red blood cells of most women. These blood cells are considered Rh positive. Some women have red blood cells that do not produce Rh protein. These blood cells are considered Rh negative.
Pregnant women who have Rh-negative blood are at risk of reacting against fetal blood that is Rh positive. Because a reaction can harm future pregnancies, Rh-negative women usually receive an injection of Rh immunoglobulin (RhIG) to prevent Rh-related problems after miscarriage or abortion.
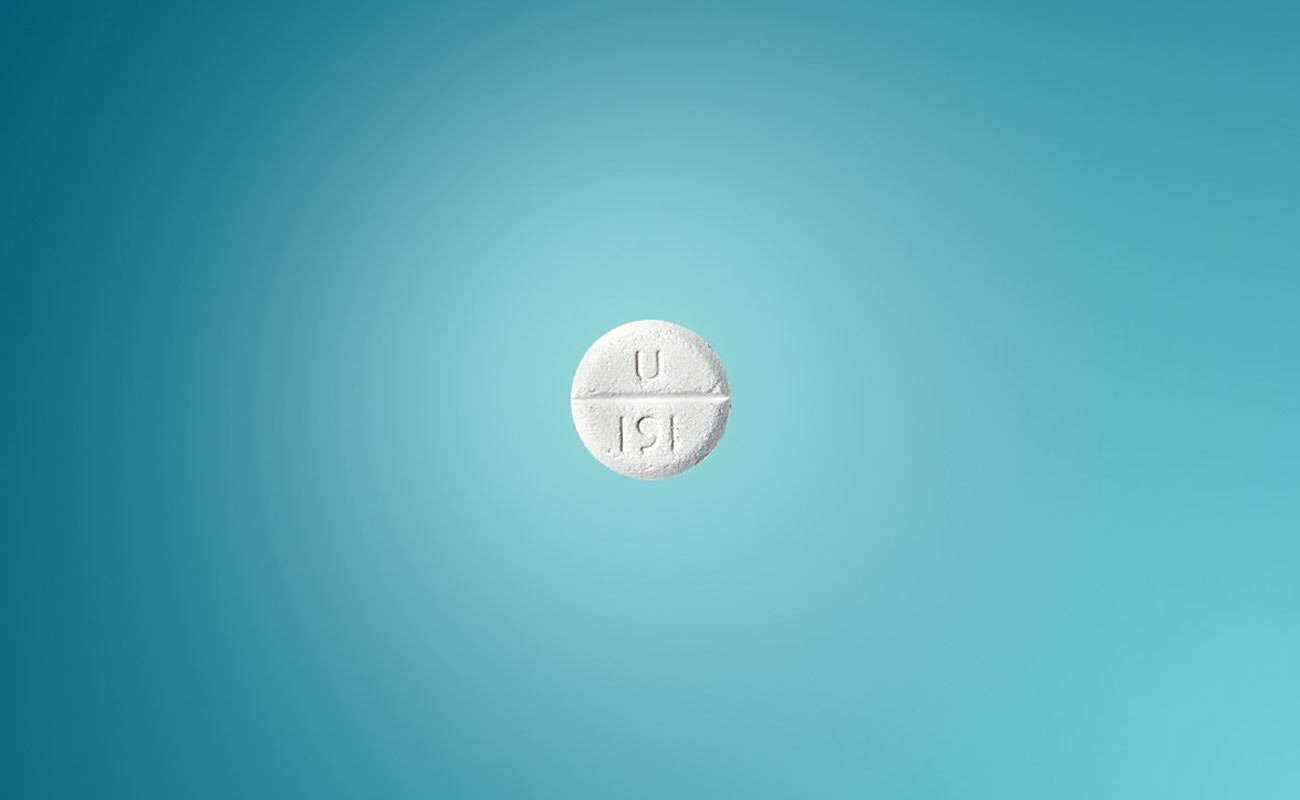
Abortions completed with medication, called medical abortions, can be performed within 64 days of gestation. Days of gestation are the number of days beginning on the first day of your last menstrual period.
Medications used to induce abortion include:
In rare instances when a pregnancy continues after the use of these medications, there is a risk that the baby will be born deformed. The risk is greater with the use of misoprostol. If the pregnancy tissue does not completely leave the body within two weeks of a medical abortion, or if a woman bleeds heavily, then a surgical procedure may be needed to complete the abortion. Approximately 2% to 3% of women who have a medical abortion will need to have a surgical procedure, usually suction dilation and curettage (D and C), also called vacuum aspiration.
Aspiration is a surgical abortion procedure performed during the first 6 to 16 weeks gestation. It is also referred to as suction aspiration, suction curettage, or vacuum aspiration. Your abortion provider will give you medication for pain and possibly sedation. You will lie on your back with your feet in stirrups, and a speculum is inserted to open the vagina.
A local anesthetic is administered to your cervix to numb it. Then a tenaculum (surgical instrument with long handles and a clamp at the end) is used to hold the cervix in place for the cervix to be dilated by absorbent rods that vary in size.
The rods may also be put in a few days prior to the procedure. When the cervix is wide enough, a cannula, which is a long plastic tube connected to a suction device, is inserted into the uterus to suction out the fetus and placenta.
The procedure usually lasts 10-15 minutes, but recovery can require staying at the clinic for a few hours. Your doctor will also give you antibiotics to help prevent infection.
Side effects and risks of suction aspiration
Common side effects of the procedure include cramping, nausea, sweating, and feeling faint. Less frequent side effects include possible heavy or prolong bleeding, blood clots, damage to the cervix and perforation of the uterus.
Infection due to remaining tissue or infection caused by an STD or bacteria being introduced to the uterus can cause fever, pain, abdominal tenderness and possibly scar tissue. Contact your healthcare provider immediately if your side effects persist or worsen.

Dilation and evacuation is a surgical abortion procedure performed after 16 weeks gestation. In most cases, 24 hours prior to the actual procedure, your abortion provider will insert laminaria or a synthetic dilator inside your cervix. When the procedure begins the next day, your abortion provider will use a tenaculum to keep the cervix and uterus in place and cone-shaped rods of increasing size are used to continue the dilation process.
A numbing medication will be used on the cervix. A shot may be given before the procedure begins to ensure fetal death has occurred. A cannula (long tube) will then be inserted to begin removing tissue away from the lining.
Then, using a curette (surgical instrument shaped like a scoop or spoon), the lining is scraped to remove any residuals. If needed, forceps may be used to remove larger parts. The last step is usually a final suctioning to make sure the contents are completely removed.
The procedure normally takes between 15-30 minutes. The fetal remains are usually examined to ensure everything was removed and that the abortion was complete. An antibiotic will be given to help prevent infection.
What are the side effects and risks of dilation & evacuation?
Common side effects include nausea, bleeding, and cramping which may last for two weeks following the procedure.
Although rare, the following are additional risks related to dilation and evacuation: damage to uterine lining or cervix, perforation of the uterus, infection, and blood clots. Contact your healthcare provider immediately if your symptoms persist or worsen.
The dilation and extraction procedure is used after 21 weeks gestation. The procedure is also known as D & X, Intact D & X, Intrauterine Cranial Decompression, and Partial Birth Abortion.
Two days before the procedure, laminaria is inserted vaginally to dilate the cervix. Your water should break on the third day and you should return to the clinic. The fetus is rotated and forceps are used to grasp and pull the legs, shoulders, and arms through the birth canal.
A small incision is made at the base of the skull to allow a suction catheter inside. The catheter removes the cerebral material until the skull collapses. The fetus is then completely removed.
The availability of any procedure used in the third trimester is based on the laws of that state.
What are the side effects and risks related to dilation and extraction?
The side effects are the same as dilation and evacuation. However, there is an increased chance of emotional problems from the reality of more advanced fetal development. Contact your healthcare provider immediately if your symptoms persist or worsen.
Below is a description of the immediate abortion risks:
Pelvic Infection: Germs (bacteria) from the vagina or cervix may enter the uterus during the abortion and cause an infection in the pelvic region. Antibiotics can treat infections but, in rare cases, a repeat suction abortion, hospitalization and/or surgery may be required.
Incomplete abortion risks: An incomplete abortion outlines that part of the fetus, or other products of pregnancy (placenta), may not drain completely from the uterus, requiring further medical procedures. This may result in infection and bleeding.
Blood clots in the uterus: Blood clots that produce severe cramping can also occur. The clots usually are removed by a repeat surgical abortion procedure.
Heavy bleeding: Some bleeding is typical after an abortion. Heavy bleeding (hemorrhaging) is not common and may be treated by repeat suction (surgical abortion), medication or, rarely, surgery. Be sure to ask your doctor to explain heavy bleeding and what to do if it happens.
Cut or torn cervix: The opening of the uterus (cervix) may be torn because the abortionist must stretch it open to allow medical instruments to pass into the uterus during surgical abortion procedures.
Puncture/Tear of the wall of the uterus: A medical instrument can cut through the wall of the uterus during a suction abortion procedure. Perforation can lead to infection, heavy bleeding or both, depending on the severity of the cut. Surgery may be required to repair the uterine tissue, and in serious cases, a hysterectomy (surgical removal of the uterus) may be required.
Anesthesia-related complications: As with other surgical procedures, anesthesia increases the risk of complications associated with abortion. Due to these riskd, many surgical abortion procedures are completed without benefit of anesthesia which can entail a great deal of physical pain to the woman.
Rh Immune Globulin Therapy: Genetic material found on the surface of a woman’s red blood cells are known as the Rh Factor. If a woman and her fetus have different Rh factors, she must receive medication to prevent the development of antibodies that would endanger future pregnancies.
Scar tissue on the uterine wall. A surgical abortion can result in the growth of scar tissue in the uterus, a condition known as Asherman’s syndrome. This can lead to abnormal, absent or painful menstrual cycles, future miscarriages and infertility.
Abortion Risk – Impact on Future Pregnancies:
Complications associated with an abortion, or having multiple abortions, may make it difficult to have children in the future.
In addition, some research suggests a possible link between abortion and an increased risk of the following in future pregnancies:

Because every person is different, one woman’s reaction to an abortion will certainly be different from another’s at a spiritual, emotional, psychological or physical level. These impacts can vary over time, depending on the mental health of the post-abortive person.
After an abortion, a woman may have both positive and negative feelings regarding her choice, even at the same time. It’s typical to feel instant relief due to the fact that the procedure is over and that she is no longer in an unplanned pregnancy. However, after a few months, this relief can be replaced with many other emotional reactions.
One woman may feel sad that she was in a position where all of her choices were difficult ones. She may feel emotionally sad about ending her pregnancy. She may also experience a sense of emptiness or guilt, wondering whether or not her decision was correct.
Some women who describe these feelings find they go away with time. Others find them more difficult to overcome as time advances.
Certain factors can increase the chance that a woman may have a difficult adjustment to an abortion.
ramahinternational.org, americanpregnancy.org, drugs.com, webmd.com, steadyhealth.com, livestrong.com
Submit Comment